Iron Deficiency in Autism
-
Iron deficiency is the most prevalent micronutrient deficiency in the world, affecting about 2 billion people, particularly mothers and children
-
Iron deficiency is the primary cause of anaemia, affecting roughly one-quarter of the world's population.
-
Iron deficiency is the second most preventable cause of mental retardation in the world.
-
Iron deficiency during pregnancy leads to iron deficiency in the neonate
-
Iron deficiency during pregnancy increases the risk for preterm labour, low birth weight and increased infant mortality.
-
Iron deficiency in children is associated with developmental delay and behavioural disorders
-
Iron deficiency in children is associated with lower verbal intelligence, attention and concept learning
-
Iron deficiency in children is a common cause of hypermobility - a common problem in ASD
-
Iron deficiency in children is also a cause of restless leg syndrome - a common problem in ASD
-
Iron deficiency in children can cause epilepsy a very common problem in ASD
-
More than 80% of children with ASD have been found to be iron deficient at time of assessment
Role of iron in brain development
Iron loading of the brain, occurs predominantly in the last trimester of foetal growth. The brain is highly susceptible to iron deficiency during the late foetal and early neonatal time period. Deficiency at this time is associated with altered expression of genes critical for development and function, and deficiency at this time causes neurocognitive dysfunction, which may continue even after iron stores have become replete.
Iron deficiency in the mothers results in decreased oxygen transport, which decreases as the haematocrit and haemoglobulin concentration of the mother's blood decreases. This is then further exacerbated by reduced iron in the foetus, leading to further reduction in oxygen transport across the placenta and reduced availability of oxygen to the developing foetus due to reductions in foetal haemoglobin and foetal haematocrit.
Iron deficiency has been associated with poorer voice recognition in the neonate, and whilst infants with iron sufficiency can be shown electrophysiologically to recognize their mother's voice, children with fetal-neonatal iron deficiency did not. This was associated with poorer auditory recognition memory at 2 months of age and is consistent with effects of iron deficiency on the developing hippocampus in the brain.
Iron deficiency in utero affects the development of cerebellar Purkinje cells, specific neurons involved in fine-tuned motor control, balance, proprioception, and the vestibular-ocular reflex (VOR), a reflex essential in eye-tracking of an object when the head is moved. Several reports have indicated that there are 35-95% fewer Purkinje cells in the cerebrum of ASD brains in comparison to neurotypically normal brains. Damage to this area of the brain has been associated with a range of conditions including ataxia, intention tremors, stiff or high stepping gait, lack of awareness of foot position and a general inability to judge distance and space. Reduced VOR has implications for reading and focusing and as such causes problems in focusing and reading of fine print.
Iron deficiency has been associated with lower production of brain-derived neurotrophic factor, an important factor involved in the development of learning, memory and behaviour (Yusrawati etal, 2018)
Decreased iron concentration in the brain is associated with irritability, apathy reduced ability to concentrate and with various other deficiencies in cognition. Iron deficiency in the brain is also associated with deficit in language capability. In addition, Iron deficiency is associated with hypomyelination of nerves, thus reducing the maturation of rapid impulse transmission along nerves.
Iron deficiency also correlates with a decreased nerve conduction velocity (Kabakus etal, 2002), and reduced energy production in Krebs cycle, with the result that decreases in iron are associated with decreased mini mental score a measure of IQ (Mangialasche etal, 2015)
Iron Deficiency in the fetus
Iron deficiency is very common in pregnancies (40-50% as determined by IDA), however, not all iron mothers with ID have children with ASD. Further the difference in iron levels in the serum of kids +/- ASD is very little. Low iron intake, when combined with advanced age of the mothers, resulted in a five-fold increased risk of having an ASD child (Schmidt 2014).
Brain accumulation of iron appears to happen primarily in utero, and uptake of iron into the brain, post weaning, is limited (63). It is critical that the developing foetus receives sufficient iron for neuronal development in the brain and that there is sufficient iron for the neonate to have adequate stores to last for the first six months of life. This is because the immature neonatal gut is not developmentally mature and as such cannot regulate the uptake of iron (Radlowsky and Johnson 2013), and additionally breast milk is very low in iron content. Maturation of the gut will be further compromised if the mother is vitamin B12 deficient as melatonin production is reduced in B12 deficiency and melatonin secreted by the mammary gland is required for gut maturation. The majority of the fetal liver stores (66%) are acquired in the last one-third of pregnancy and so infants born prematurely with a low birth weight are at greater risk of iron deficiency. Infants who are born to iron deficient mothers are still found to be abnormally low in iron 9 months after birth, even if provided adequate dietary iron (Radlowsky and Johnson 2013). Iron deficiency at this time creates other problems as iron is preferentially used for production of haemoglobin, and in iron deficiency, iron is sequestered for the production of hemoglobin and so non-heme tissues such as skeletal muscle, the heart and the brain will become iron deficient a long time before overt anaemia is obvious (Rao and Georgieff, 2002). Once born, infant brain iron levels decrease in the first 6 months of life, which roughly equates to the onset of myelination. The most sensitive period (and hence the period that can cause the most irreversible damage) is the period between 0 and 24 months of age. Iron deficiency in this period is correlated with poor auditory recognition memory, delayed cognitive development and poor response to external stimuli.
During pregnancy the mother sacrificially loads up the foetus with the result that many women can become iron deficient during pregnancy. Children born to mothers with low serum ferritin tend to have low serum ferritin as well, and that there is a positive correlation between maternal serum ferritin and the resultant iron reserves in the children (Gaspar etal, 1993; Jaime-Perez etal, 2005; Shao etal, 2012; Lee et al, 2016). Iron loading of the foetus occurs progressively during foetal development and depends upon gestational age, and also the iron levels of the mother, hence the shorter the pregnancy and the lower the iron in the mother, the lower the iron in the foetus.
From Siddapathi etal, 2007
Iron deficiency is associated with lower activity of an important enzyme, aconitase and in the elderly low aconitase activity is associated with lower mini mental score estimation
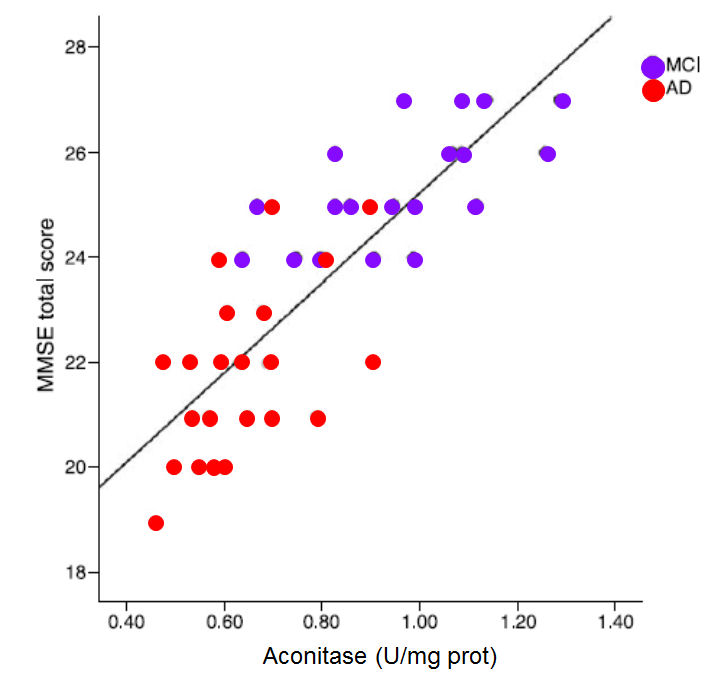
MMSE score against the activity of the enzyme aconitase (Figure. Data from Mangialasche etal,2015)
Iron Deficiency in autism
It has been known for some time that the level of iron in the brains of autistic children is much lower than in normal individuals (Bener 2017; Latif etal, 2002,; Drosman etal, 2006, 2007, Heuguner etal, 2012; Reynolds etal, 2012; Youssef etal, 2013; Sidrak etal, 2014). Iron deficiency was associated with lower haemoglobin, haematocrit, and MCV values (Gunes 2017), with a negative correlation between lower haematocrit levels and degree of symptomatology (Sidra 2014). Iron deficiency in neonates has also been associated with poor emotional outcomes (Kim, 2014; Zumbrennen-Bullough 2004), recognition memory (Geng 2015), poor neural maturation (Armin 2010; Choudhury 2015; Armony-Sivan 2004). Iron is essential for learning and memory, and both the cholinergic and glutamatergic neurotransmission pathways are regulated by iron, and play a huge role in memory performance (Han 2015; Rodlowski and Johnson, 2013) and in the production of myelin by myelin-producing oligodendrocytes (Rosato-Siri 2017; Roth 2016).
Function of Iron in the body
For many years, it was thought that iron was solely involved as part of the structure of the heme molecule such as in the structure in hemoglobin. More recently it has been recognized as an important factor in the activity of iron sulphur proteins, such as aconitase, succinate dehydrogenase, and more recently gamma-aminobutyrate amino transferase (GABA-AT) and lipoate synthase. Iron is critical for myelination of nerve cells, and lack of myelination causes slower neuronal conduction, abnormal reflexes in children, and deficits in auditory and visual function (Armin etal, 2010). Iron deficiency has also been associated with poorer language and global IQ, and social and attention problems. Iron-deficiency anemia is an advanced stage of iron deficiency, however, early Iron deficiency is associated with cognitive alterations in adolescents, and with developmental delay in children. Iron deficiency is generally associated with reduced levels of the iron storage protein, ferritin and ferritin levels are significantly lower in ASD kids (28.6 ug/L +/- 22 ug/L) when compared to normal individuals (152 ug/L +/- 142 ug/L). Deficiency of activity of Fe-S proteins has been shown to result in lower energy output in Krebs cycle and the electron transport chain, and also lack of emotional control due to lack of activity of GABA-AT, with increased anxiety. Increased levels of GABA are characteristic of iron deficiency, presumably due the lack of function of GABA-aminotransferase, an iron-sulphur protein, whose production is limited in iron and vitamin B12 deficiency.
Iron is required for appropriate behavioral organization. Iron deficiency results in poor brain myelination and impaired monoamine metabolism. Glutamate and GABA homeostasis is modified by changes in brain iron status. Such changes not only produce deficits in memory/learning capacity and motor skills, but also emotional and psychological problems. An accumulating body of evidence indicates that both energy metabolism and neurotransmitter homeostasis influence emotional behavior, and both functions are influenced by brain iron status.” (Kim and Wessling-Resnick, 2014)
Iron has a critical role in the formation of the myelin sheath around neurons, and iron deficiency in mothers has shown a higher incidence of conditions such as ASD, and has also been associated with irreversible alterations in myelin. Iron deficiency in the brain precedes the signs of iron deficiency in RBC production. Serum ferritin levels below 76 ug/L are associated with abnormalities in neonatal recognition memory, and neuronal processing. Further, a recent study has shown that lower iron levels (as judged by serum ferritin) are associated with decreased brain activity and lower energy expenditure, as well as a reduced heart rate. Iron is known to be critical in neurodevelopment, and fetal iron deficiency has been shown to result in acute brain dysfunction, with long-lasting abnormalities even after repletion. Lower iron is also associated with restless leg syndrome and febrile seizures, which are common in children with ASD (Sherjil etal 2010; Fallah etal, 2014; Gillberg etal, 2017; McCue etal, 2016; Hara 2007). Seizure rates were increased in children on soy infant formula, presumably due to the lower iron content. Iron deficiency is associated with a greater risk of headache, particularly if blood pressure is elevated. Worryingly, iron deficiency is still be defined by clinicians in term of iron deficiency anemia, and values of 12 or 15 ug/L ferritin being commonly used to assign deficiency. Thus, children who have many of the signs assigned to iron deficiency, such as reduced cognition, developmental delay, depression, poor neuronal processing, anxiety, migraine headaches, restless leg syndrome and febrile seizures, are not being treated for iron deficiency due to clinicians sticking to archaic, anemia defined, definitions of iron sufficiency. Our studies have shown reduced energy production by aconitase and succinate dehydrogenase when serum ferritin levels drop below 70 ug/L. This reduced energy production can be seen by the massive increase in energy lost in the form of citrate as iron (as measured by ferritin) levels drop. Our studies have shown that as ferritin levels drop from 70 to 20 ug/L (seen not deemed as iron deficient by most pathology labs) up to 9 times the amount of citrate is lost to those who are iron replete. This means that effective energy consumption by the brain will also drop. Such energy loss, if extrapolated "planet-wise" is catastrophic environmentally.
Iron deficiency has been shown to cause iron deposition in white matter in the brain and in oligodendrocytes (mylein producing cells). The dysregulation of iron metabolism ultimately leads to neurological, behavioural and nociceptive impairments. Iron deficiency can lead to anemia, changes in cognitive performance, emotions, behavior, reduced exercise capacity, and myocardial functional and structural changes (Fava etal, 2019; Jankowaska et al 2011).
Iron Deficiency and Hypermobility
Iron has a critical role in cross-linking collagen fibers thereby increasing their tensile strength and reducing their stretchibility. Lack of iron has been associated with hypermobility, a condition common in autism (Glans etal, 2017; Cederlof etal 2016; Sinibaldi et al, 2015; Casanova etal, 2018; Baeza-Velasco etal, 2018)
Determination of Iron Deficiency
One of THE biggest problems in determining iron deficiencies in the mothers revolves around the definition of iron deficiency. Generally Iron deficiency has not been related to biochemical iron deficiency, but rather to some arbitrary value correlating ferritin values with anaemia. These arbitrary values vary greatly depending upon the country in which the measurements are taken, and do not reflect various biochemical parameters whose values measure markers of iron deficiency. Thus, Iron deficiency as judged by haematological parameters occurs at around 15-20 ug/L ferritin in adults, however, metabolically iron deficiency can be observed when ferritin values drop below 70 ug/L and evidence of altered cell metabolism occurs when ferritin drops below 100 ug/L. Further, there appears to be a general ignorance in the medical profession of the role of iron in the body, and what effect lowered Haemoglobin and haematocrit have on oxygen carrying capacity of the blood, nor the massive reduction in energy seen in Krebs cycle as a result of decreased activity of the enzyme aconitase, when ferritin levels drop below 60 ug/L. This observation would support the contention of several workers that serum ferritin below 74 ug/L is indicative of abnormalities in neonatal recognition memory, in reflexes and in the myelin-dependent speed of neuronal processing (Georgieff, 2017, Geng etal, 2015; Armony-Sivanetal, 2004; Armin et al, 2010)
Definitions of iron deficiency also vary from country to country, with a cut-off of 12 ug/L in Indonesia (Yusrawati etal, 2018), 12 ug/L in Brazil (de Sa etal, 2015). This is further complicated by the definitions associated with iron deficiency such as levels of haemoglobin and haematocrit, both of which are different from biochemical evidence of iron deficiency. Thus, iron deficiency can be categorized into three main types, iron deficiency with anaemia, which relates purely to the number of Red Blood Cells, biochemical iron deficiency without anaemia, in which biochemical parameters of iron deficiency can be measured, or iron sufficiency. Of these, iron sufficiency appears occur above 70 ug/L ferritin.
A recent summary of guidelines for management of iron deficiency, world-wide, recommended serum ferritin values should be above 100 ug/L (Peyrin-Biroulet etal, 2015; Fava eta; 2019). Recently, the American Gastroenterological Society has set a new minimum for defining iron deficiency of 45 ug/L for ferritin (Ko etal, 2020).
Resolving Iron Deficiency in Autism
Iron
deficiency is extremely common in ASD and this needs to be addressed if the
child is going to have any chance of normal development. For neurotypically normal development
large quantities of iron are required for the process of myelination of the
brain and peripheral nervous system. Estimates are 7 mg/day for children 1 to 8
years old. This estimate is of bioavailable iron, NOT of iron in the supplement.
It is best to introduce iron containing meats, such as beef or chicken liver,
clams, mollusks or mussels or oysters >> beef, lamb goat, deer, bison, sardines
turkey, all of which have much higher iron contents than chicken or pork.
Non-meat sources of iron are extremely poorly absorbed, even despite this
studies have shown that
6
mg/kg/24 h ferrous sulphate when given orally is able to restore normal
nerve conduction velocities in children with iron deficiency (Kabakus etal,
2002). A
recent study using oral iron-bisglycinate given at 3 mg/kg (90 mg/30 kg child)
resulted in a modest increase in serum ferritin from 20 ug/L to 40 ug/L after 45
days (Name etal, 2018), supporting the observations that oral absorption of non-heme
iron is very inefficient. One study suggested that there is actually more iron
that is available from the rusting of an iron pot than is available from cooking
non-heme foods. Studies on iron absorption from beans suggests that oral
bioavailabiity of iron may be as little as 0.4% (
Junqueira-Franco etal, 2018)
Iron Deficiency and altered Thyroid Function
Iron is involved in the function of the enzyme thyroid peroxidase, and as levels of ferritin in serum drop, the activity of the enzyme becomes compromised and levels of thyroid hormone drop with an accompanying rise in TSH (Eftekhari etal, 2006), potentially making individuals with low iron hypothyroidic (Veltri et al, 2016' Li etal, 2016; Tenq etal, 2018), which would result in functional B2 deficiency (Maldonado-Araque etal, 2018). This effect would be exacerbated in pregnancy as levels of iron in the mother drop as they "feed" the foetus with iron. Such hypothyroxinemia induces by iron deficiency impairs normal brain development (Hu etal, 2016).

Resolving Iron Deficiency in Pregnant mothers
Iron deficiency is extremely common in vegetarian adults, and amongst female vegetarians, 12-79%, depending upon the study, where found to have exceedingly low serum ferritin, <12 ug/L (Pawlak etal, 2016). The prevalence of iron deficiency anaemia in pregnancy (IDAP) is estimated to be 20% globally [1] and 11–18% in Australia [2, 3.(Smith-Wade etal, 2020). Children of mothers with levels that low would be in grave danger of very low brain iron levels, and to potentially have irreversible brain damage. Studies carried out in Denmark by Milman and co-workers (2006) looked at iron deficiency in pregnant mothers and came up with the following suggestions: "80-100 mg ferrous iron/day to women having ferritin <or=30 microg/l and 40 mg ferrous iron/day to women having ferritin 31-70 mug/l. In the prevention of IDA, we suggest 40 mg ferrous iron/day to women having ferritin <or=70 microg/l. Women with ferritin >70 microg/l have no need for iron supplement." Iron availability from food sources has vastly different absorption characteristics, thus heme-iron, such as that found in red meat, and seafood, is much more efficiently absorbed than similar quantities of iron found in vegetables, particularly those containing iron-complexing/chelating molecules such as phytates. The data below is from a study comparing the uptake of iron (Fe) from heme iron (open bars) to that from non-heme iron sources (closed bars) (Hunt, 2003).
During pregnancy, there is a marked drop in ferritin levels in the mother, as firstly her blood volume increases dramatically, and secondly, the foetus starts to accumulate iron particularly in the third trimester. For this reason determination of iron sufficiency is somewhat harder during pregnancy.
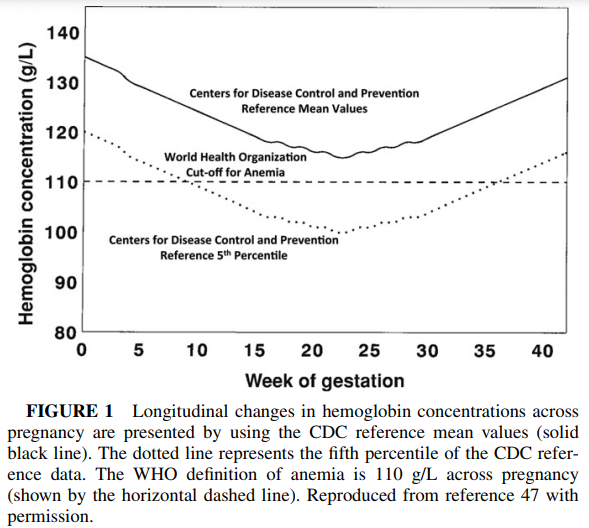
O'Brien and Ru, 2017
Associated Deficiencies in Autism
The majority of studies looking at iron deficiency in children and in autism have now addressed the likely co-deficiency of vitamin B12, however, one could assume that a diet low in iron would also be a diet low in vitamin B12. Every child that we have data for who has autism is also deficient in active vitamin B2 (FMN and FAD) and is deficient in active vitamin B12 (Adenosyl and Methyl B12), these deficiencies also have to be addressed or the child will potentially have a considerable developmental delay.
References
-
Yusrawati etal Differences in brain-derived neurotrophic factor between neonates born to mothers with normal and low ferritin. Asia Pac J Clin Nutr 2018 27: 389-392
Schmidt et al Maternal intake of supplemental iron and risk of autism spectrum disorder 2014 PMID 25249546
Radlowski and Johnson Perinatal iron deficiency and neurocognitive development Front Hum Neurosci 2013 7, 585
Rao and Georgieff Perinatal aspects of iron metabolism https://www.ncbi.nim.nih.gov/pubmed/12477276
Amin etal In utero iron status and auditory neural maturation in premature infants as evaluated by auditory brainstem response. PMID 19939407
Hare etal, 2013 A delicate balance: Iron metabolism and diseases of the brain... PMIC 3715022
Kwik-Uribe etal, 2000 Chronic marginal iron intakes during early development in mice result in persistent changes in dopamine metabolism and myelin composition.PMID 11053527
Choudhury etal 2015 Latent iron deficiency at birth influences auditory neural maturation in late preterm and term infants PMID 26310540
Armony-Sivan etal 2004 Iron status and neurobehavioral development of premature infants PMID 15318248
Wenger etal, 2017 Effect of iron deficiency on simultaneous measures of behavior, brain activity and energy.. PMID 28784049
Kim and Wessling-Resnick 2014 Iron and Mechanisms of Emotional Behaviour. PMC 4253901
Zumbrennen-Bullough etal 2014 Abnormal brain iron metabolism in Irp2 deficient mice is associated with mild neurological and behavioral impairments PMID 24896637
Georgieff 2008 The role of iron in neurodevelopment: fetal iron deficiency and the developing hippocampus PMID PMC2711433
Sherjil etal 2010 Iron deficiency anaemia - a risk factor for febrile seizures in children PMID 22338422
Fallah etal 2014 Iron deficiency and iron deficiency anemia in children with first attack of seizure and on healthy control group.... PMC PMC4135276
Gillberg etal 2017 Febrile seizures and epilepsy: Association with autism and other neurodevelopmental disorders in the child....... PMID 28754226
McCue etal 2016 Prevalence of non-febrile seizures in children with idiopathic autism spectrum disorder and their unaffected siblings....... PMID 27894273
Kabakus etal 2002 Reversal of iron deficiency anemia-induced peripheral neuropathy by iron treatment of children with iron deficiency anemia. PMID: 12200980
Mangialasche etal, 2015 Lymphocytic mitochondrial aconitase activity is reduced in Alzheimer's disease and mild cognitive impairment. PMID: 25322927
Pawlak etal, 2016. Iron status of Vegetarian Adults: A literature review.
Hara 2007 Autism and epilepsy: a retrospective follow-up study PMID 17321709
Fallah etal 2016 Evaluation efficacy of ferrous sulfate therapy on headaches of 5-15 years old iron deficient children with migraine PMC
Giulivi et al Mitochondrial dysfunction in autism. J. Am. Med Assoc 2010 304: 2387-2396
Chauhan etal Brain region-specific deficit in mitochondrial electron transport chain complexes in children with autism. J. Neurochem. 2011 117: 209-22
Tang et al Mitochondrial abnormalities in temporal lobe of autistic brain. Neurobiol Dis 2013 54: 349-361
Napoli et al Deficits in bioenergetics and impaired immune response in granulocytes from children with autism. Pediatrics 2014 133:e1405-10
Zumbrennen-Bullough; et al. Abnormal brain iron metabolism in Irp2 deficient mice is associated with mild neurological and behavioural impairment. PloS One 2014 e98072 PMC 4045679
Sherjil et al Iron deficiency anaemia - a risk factor for febrile seizures in children 2010 PMID 22338422
Westmark Soy infant formula and seizures in children with autism: a retrospective study. 2007 PMID 24622158
Sa et al. Anemia in pregnancy: impact of weight and in the development of anemia in the newborn. Nutr Hosp 2015 32:2071-2079
Gaspar et al. Relationships between iron status in pregnant women and their newborn babies.. Acta Obstet Gynecol. Scand. 1993 72:5234-7
Jaime-Perez et al. Sub-optimal fetal iron acquisition under a maternal environment. Arch Med Res. 2005 36: 598-602
Shao et al. Maternal serum ferritin concentraion is positively associated with newborn iron stores in women with low ferritin status in late pregnancy. J. Nutri. 2012 142:2004-9
Lee et al. Prevalence of anaemia and associations between neonatal iron status, hepcidin and maternal iron status among neonates born to pregnant adolescents. Ped Res. 2016 79:42-8
Kabakus et al, Reversal of iron deficiency anemia-induced peripheral neuropathy by iron treatment of children with iron deficiency anemia. J Trop Ped 2002 48: 204-9
https://nutritionovereasy.com/2015/05/cast-iron-pans-can-increase-your-iron-intake/
Brittin HC, Nossaman CE. Iron content of food cooked in iron utensils. J Am Diet Assoc. 1986;86:897–901
Junqueira-Franco etal, Iron absorption from beans with different contents of iron, evaluated by stable isotopes. PMID 29779806
Eftekhari etal The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls. https://www.ncbi.nlm.nih.gov/pubmed/16500878
Veltri etal, 2016 Prevalence of thyroid autoimmunity and dysfunction in women with iron-deficiency in early pregnancy... https://www.ncbi.nlm. nih.gov/pubmed/27450694
Li etal, 2016 The relationship between iron deficiency and thyroid function in Chinese women during early pregnancy https://www.jstage.jst.go.jp/article/jnsv/62/6/62_392/_article
Tenq etal, 2018 Iron deficiency may predict greater risk for hypthyroxinemia: A retropective cohort study of pregnant women in China https://www.ncbi.nlm.nih.gov/pubmed/29968513
Maldonado-Araque etal, 2018 Iron deficiency is associated with hypothyroxinemia ... https://www.ncbi.nlm.nih.gov/pubmed/29700318
Yu et al Iron deficiency, an independent risk factor for isolated hypothyroxinemia in pregnant ...... https://www.ncbi.nlm.nih.gov/pubmed/25599388
Hu etal Perinatal iron deficiency-induced hypothyroxinemia impairs early brain development https://www.ncbi.nlm.nih.gov/pubmed/27231981
Name etal Iron Bisglycinate Chelate and Polymaltose Iron for the Treatment of Iron Deficiency Anemia: A Pilot Randomized Trial PMID 6416187
Milman et al. Body iron and individual iron prophylaxis in pregnancy - should the iron dose be adjusted according to serum ferritin. Ann Hematol. 2006 85: 567-73
Ko etal. AGA Clinical Practise guidelines.... 2020 Gastroenterology 159: 1085-1094
Fava et al. Heart failure and iron deficiency 2019 https://www.ncbi.nlm.nih.gov/pubmed/30821294
Jankowska et al Iron deficiency predicts impaired exercise capacity in patients with cystolic chronic heart failure https://www.ncbi.nom.nih.gov/pubmed/22041326
https://www.thewomens.org.au/images/uploads/fact-sheets/Iron-Infusion-0718.pdf
Hunt, JR. 2003 Bioavailability of iron, zinc, and other trace minerals from vegetarian diets. Am J Clin Nut, 78: 633S-9
Glans etal, 2017 Generalized joint hypermobility and neurodevelopmental traits in a no-clinical adult population. BJPsych Open 2017 27, 236-242
Baeza-Velasco etal. Joint hypermobility and the heritable disorders of connective tissu: Clinical and empirical evidence of links with psychiatry. Gen Hosp Psychiatry 2015, 37, 24-30
Cederlof etal Nationwide population-based cohort study of psychiatric disorders in individuals with Ehlers-Danlos syndrome or hypermobility sydnrome and their siblings. BMC Psychiatry 2016; 4, 16-207
Sinibaldi et al. Psychopathological manifestations of joint hypermobility and joint Hypermobility Syndrome/Ehlers-Danlos syndrome, hypermobility type: The link between connective tissue and psychological distress revised. Am J Med Genet 2015; 169C 97-106
Smith-Wade et al. BMC Pregnancy and Childbirth (2020) 20:665
World Health Organization. Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva; World Health Organization; 2012.
Khalafallah A, Dennis A, Bates J, et al. A prospective randomized, controlled trial of intravenous versus oral iron for moderate iron deficiency anaemia of pregnancy. J Intern Med. 2010;268:286–95.
Zhou SJ, Gibson RA, Crowther CA, Baghurst P, Makrides M. Effect of iron supplementation during pregnancy on the intelligence quotient and behavior of children at 4 y of age: long-term follow-up of a randomized controlled trial. Am J Clin Nutr. 2006;83:1112–7.
Casanova etal. A cohort study comparing women with autism spectrum disorder with and without generalized joint hypermobility. Behav Sci 2018, 17; 8:35
Baeza-Velasco etal Autism, joint hypermobility-related disorders and pain. Front Psychiatry 2018; 7, 9; 656
Russell etal. Symptoms of restless leg syndrome in biological caregivers of children with autism spectrum disorders. J.Clin. Sleep Med 2017 13: 105-113
Horiuchi etal. The diagnosis and treatment of sleep and neurodevelopmental disorders; Seishin Shinkeigaku Zasshi 2016; 118, 410-416
Ming etal. Autism spectrum disorders, attention deficit/hyperactivity disorder, and sleep disorders. Curr Opin Pulm Med 2009 15; 578-84
Kotagal S. Treatment of dssomnias and parasomnias in childhood. Curr Treat Options Neurol 2012; 14: 630-49
Belousova and Zavadenko Epilepsy and autism spectrum disorders in children. Zh Neverol Psikhiatr Im S S Korsakova 2018; 118; 80-85
Keller etal. Autism, epilepsy, and synaptopathies: a not rate association. Neurol Sci 2017 38; 1353-1361
Richard etal. Features of the broader autism phenotype in people with epilepsy support shared mechanisms between epilepsy and autism spectrum disorder. Neurosci Biobehav Rev 2017; 75; 203-233
Gillberg etal. Febrile seizures and epilepsy: association with autism and other neurodevelopmental disorders in the child and adolescent twin study in Sweden. Pediatr Neurol. 2017 74; 80-86.e2
Christensen etal Risk of epilepsy and autism in full and half-siblings- A population-based cohort study. Epilepsia 2016, 57; 2011-2018
O'Brien and Ru, 2017 Iron status of North American pregnant women: an update on longitudinal data and gaps in knowledge from the United States and Canada.Am J Clin Nutr 2017;106(Suppl):1647S–54S.
Copyright © 2014 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited