"Nexus Theory™"
In the preceding sections on Iron, Vitamin B12, Vitamin B2 and Vitamin D we discussed how deficiencies in each of these factors are associated with the development of Autism, and identification of such deficiencies may help in the treatment and prevention of the condition. The possibility exists that at some stage in development, all of these factors "come together" at some point, and as such the condition has a much higher probability of occurring if some or all of the factors are involved in a unique developmentally important reaction or functional activity. Such a meeting point would be regarded as a "Nexus". According to the "Nexus Theory™", proposed by Dr Russell-Jones, the deficiencies outlined in the relevant sections come together in a central point, vertix, or Nexus. This point of convergence involves the final step in activation of the pro-hormone form of vitamin D (calcidiol, 25-hydroxy-vitamin D) to the biologically active form of vitamin D (calcitriol, 1,25-dihydroxy-vitamin D). This Nexus involves the interaction of three different enzymes in a three enzyme complex, CYP27B1 (25-hydroxyvitamin D3 1-alpha-hydroxylase), Adrenodoxin (an Iron-sulphur protein) and Adrenodoxin reductase (an NADPH/.FAD enzyme). A corollary of the theory is that a deficiency in the amount of 1, 25-dihydroxy vitamin D in combination with the deficiencies that cause the vitamin D deficiency (iron, B2 and B12) would dramatically affect the development of both the foetus and the new-born child. Since both active vitamin D and melatonin (a methylation product) are required for induction of neuronal stem cells to become myelin-producing oligodendrocytes, the condition would become even more "serious" as levels of functional B12 were reduced. Given that maintenance of myelin-producing oligodendrocytes in adults, the theory would be equally applicable to treatment of Alzheimer's Disease.
Vitamin D and the "Nexus Theory™"
Clearly anything that reduces circulating amounts of 25-hydroxy vitamin D, will have a direct impact on the ability of the fetus and newborn to make the biologically active form of vitamin D, 1,25-dihydroxy vitamin D, and as such will have an effect under the "Nexus Theory™". Hence the use of high SPF cosmetics by the mother or gestation that is predominantly in the winter months, or basic lack of sun-exposure of the mother during pregnancy, will reduce the circulating levels of vitamin D of the mother, and hence the amount of vitamin D that gets to the foetus. In this regard, the SPF value of women's cosmetics has increased from products with no added SPF factors, to products now "boasting" SPF values over 60, over the past 20 or so years, paralleling the increased rate of autism seen in the more affluent countries, such as USA, UK, South Korea, and Australia.
Similarly mutations in the gene coding for the Cytochrome P450 enzyme, CYP27B1 (the enzyme that "activates" vitamin D) could potentially reduce the rate and ability to convert what circulating 25-OHD (calcidiol) there is into the active form of the hormone, 1,25 DiOHD (Calcitriol). Such mutations are much more common in ASD individuals than in the normal population, particularly rs4646536, rs703842, and rs10876994, and would be more detrimental if multiple mutations are present in the gene (something that is relatively common in ASD) (Kawelvski etal, 2016). In addition, mutations in CYP24A1 that increase the inactivation of 1,25 diOHD will also reduce the available vitamin. Slightly increased frequencies are seen in the CYP24A1 variants, rs7975232 and rs2248359 in autistic individuals.
|
|
|
|
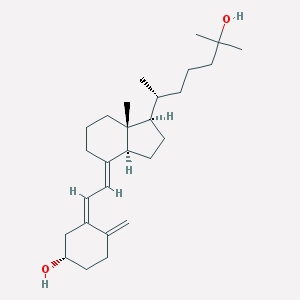
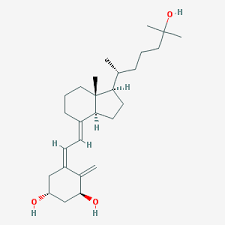
Calcidiol => |
Calcitriol |
|
|
|
|
CYP27B1 - 25-hydroxyvitamin D3 1-alpha-hydroxylase
Note the Heme Structure in the center of the enzyme |
|
Low vitamin D has also been associated with increased weight gain and diabetes, two common predisposing factors seen in mothers of autistic children.
Adrenodoxin and the Nexus Theory™
Adrenodoxin acts in concert with CYP27B1 in the
activation of vitamin D. The activity of the enzyme (Adrenodoxin) is helped by, and as such is dependent upon, the iron-sulphur
co-factor in the active site of the enzyme (see the cartoon below). Dissociation of iron-sulphur processes, such as those
found in Adrenodoxin, has been
observed when serum ferritin levels
drop below 70 ug/L. Low iron has been associated with delayed mental
development, and is commonly seen in autistic children, whose levels are commonly
found to be lower than those found in normally developing children. Lower iron
(ferritin) has also been associated with lower vitamin D levels in female
athletes (Malczewska-Lenczowska
et al, 2018)
Generation of the sulphur atom in the iron-sulphur
protein comes with the movement of the sulphur, originally occurring in dietary
methionine into the sulphation cycle. Such movement, though, is dependent upon
generation of high levels of S-Adenosylmethionine, and as such, will be lower as
levels of active vitamin B12 decrease. Apart from its role in the generation of
iron-sulphur complexes, vitamin B12, through its role in methylation, also
controls the levels of CoQ10, creatine and ultimately acetylcholine, an
important neurotransmitter in the brain. A deficiency of vitamin B12 has also
been associated with delayed mental and physical development. Lower vitamin B12 levels have
also been found in obesity and diabetes, two of the associative factors for
giving birth to a child with autism.
Adrenodoxin (also called Ferredoxin).
Note the Iron-sulphur cluster in the center of the molecule
Adrenodoxin Reductase and the Nexus Theory™
Adrenodoxin acts together with Adrenodoxin reductase in "helping" CYP27B1 to hydroxylate 25-hydroxy vitamin D and so form 1,25 dihydroxyD (Calcitriol). It's activity is critically dependent upon two co-factors, one derived from vitamin B3 (NAPDH) and the other from activation of vitamin B2 (FAD). Mutations in CYP27B1 have been described which affect binding of Adrenodoxin and can cause rickets (Zalewski etal, 2016).As mentioned in the B2 section, production of FAD requires dietary vitamin B2, Iodine, Selenium and Molybdenum, and so inadequate intake of these four nutrients can lead to reduced production of FAD, with resultant reduction in activity of Adrenodoxin reductase, and hence lower production of 1,25 Di-hydroxy vitamin D. Insufficient Iodine is one of the two most easily preventable causes of mental retardation in children. Recent studies in Boston have shown insufficient intake of Iodine in over 50% of pregnant women admitted to maternity wards. Analysis of the hair of ASD children has show that deficiencies in Selenium (80%) and Molybdenum (50%) deficiency are very common. Reduced production of FMN and FAD from vitamin B2 eventually leads to obesity, due to the inability to burn fat, diabetes, due to the inability to burn glucose for energy, and to a deficiency in vitamin B12, due to lack of activity of methionine synthase reductase and methylenetetrahydrofolate reductase. Hence the effect of low vitamin B2 would to two-fold, not only would it reduce the activity of Adrenodoxin reductase, but though its affect on maintaining active B12 would also lead to less active Adrenodoxin.
 .
.
Adrenodoxin Reductase (also called Ferredoxin reductase).
Note the FAD molecule in the center of the enzyme
Vitamin D, brain development and the Nexus Theory™
Apart from its known function in calcium metabolism and bone metabolism, vitamin D (as 1,25-diOHD) has been shown to be a potent "neurosteroid", which plays a crucial role in the developing brain. Both CYP27B1 and CYP24A1 have been found in neural cells of the fetal brain indicating that the brain has the potential to process "incoming" 25-hydroxy vitamin D, which has been formed by the mother. Much lower levels of vitamin B12, which have been found in the brains of children with autism, plus the lack of functional vitamin B2, would mean that the ability of CYP27B1 to activate what little 25-hydroxy vitamin D is present would be severely restricted, thus leading to the poor neuronal development typical of autism.
In addition to its direct role as a "neurosteroid" the combination of low 1,25 dihydroxyvitamin D, and the reduced capacity for myelination that would occur due to lack of iron, and functional vitamin B12 and vitamin B2, combined with reduced production of the neurotransmitters hydrogen sulphide, acetyl choline, and the reduced mitochondrial energy production which accompanies Iron/B12 and B2 deficiency, would more than readily explain the delayed development that typifies autism. This would be further compromised by the greatly reduced production of the developmentally important hormone, melatonin that occurs in vitamin B12 deficiency.
Recently melatonin has been shown to induce neuronal stem cell differentiation into oligodendrocytes and neurons (Mendivinil etal, 2017), hence in B12 deficiency, with the resultant lower production of melatonin, the amount of stem cell differentiation would be reduced and so too myelination This may also explain why there is a reduction in the number of immature neurons in the amygdala region of the brain in people with ASD (Avino etal 2018).
Myelination (addition of an insulatory "sheath" to the nerves) is critically important for development of speech, cognition and emotional development, and defects in myelination have been found not only in disorders such as autism, but also in dyslexia and attention-deficit hyperactivity disorder. Destruction of the myelin-sheath has also been found in Alzheimer's disease. Production of the myelin sheath in the brain is dependent upon the action of a specific cell, the oligodendrocyte, which produces the myelin layer that "wraps" around the nerve. Myelination increases the "conduction" speed of nerves and controls how they interact. Myelination of appropriate areas of the brain has been correlated with the development of specific functions in the brain, such as development of vocabulary, reading, and many cognitive tasks.
Vitamin D (as 1,25 dihydroxyvitamin D - the active form) has a critical role in remyelination in damaged nerves and in the initial myelination of nerves, and in the processes involved in "neuronal plasticity". Oligodendrocytes (the cells that make the myelin sheath) are stimulated to produce myelin by binding active vitamin D. The myelin sheath, so elicited is a layered structure, that is composed of three main proteins, one of which is myelin basic protein. The structure of myelin basic protein is critically dependent upon methylation (and hence relies upon methyl B12) and in B12 deficiency improperly folded MBP is formed and improper myelin sheath is developed. In addition, in adenosylB12 deficiency, improper lipids are inserted into the myelin sheath once again disrupting their structure.
In summary, the "Nexus Theory™" of Autism unites the various theories of the delayed mental development seen in Autism and encompasses the data on low Vitamin D, low iron, low vitamin B12, low vitamin B2, low Iodine, low selenium and low molybdenum commonly seen in autism. A real nature and nurture combination. As such the condition would appear to be entirely preventable by adequate nutrition in the mothers, and by maintaining sufficient vitamin D. Potentially, by addressing the known metabolic deficiencies present in these children, the condition could also be largely resolvable.
Further Applications: The "Nexus Theory™" has massive implications for other neuronal conditions that involve neuronal signaling or break-down, including MS, dementia, stroke, spinal chord injuries, brain plasticity, etc, and may help to explain lack of progress in these areas and provide potential areas of future research.
Measurement of Vitamin D activation and relationship to iron, vitamin B2 and vitamin B12 as per the Nexus Theory™
In the Organic Acid Test analysis (OAT), there are various markers that correlate with functional vitamin D sufficiency (Phosphoric Acid), iron sufficiency (citric acid), vitamin B2 sufficiency (glutaric acid) and vitamin B12 sufficiency (MMA, Quinolinic Acid (QA), Homovanillic Acid (HVA), CoQ10, and Pyroglutamic acid. Correlation graph for each are plotted below,

Reduced activity of the iron-sulphur protein, aconitase, results in increased secretion of citrate (citric acid) into urine. Such reduction in activity is found when ferritin levels drop below 60 ug/litre, which is when various iron-sulphur proteins, such as adrenodoxin begin to uncouple. This drop in serum ferritin precedes the drop in Haem proteins such as Haemoglobin. Hence, iron deficiency, such as is common in conditions such as autism, would be accompanied by a reduction in the conversion of 25OHD, to 1,25diOHD, which would result in functional vitamin D deficiency, and would correlate with an increase in urinary phosphoric acid (R2 = 0.4405). Reduced serum ferritin, is also associated with the reduced activity of thyroid peroxidase, and has been associated with hypothyroxinemia in pregnancy (Hu etal, 2016; Yu etal, 2015) (See figure below). Iron deficiency has previously been associated with low vitamin D (Malczewska-Lenczowska etal, 2018)
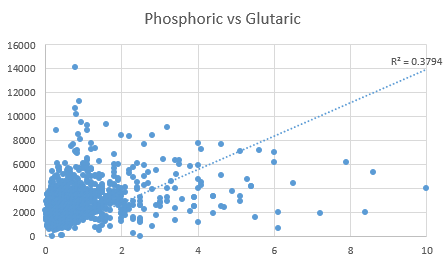
Reduction of intracellular iron, requires intracellular glutathione (GSH), which requires the action of the FAD-dependent enzyme glutathione reductase, hence in low functional B2 (as FAD), the activity of glutathione reductase is compromised, as too maintenance of functional B12 activity. In addition, Adrenodoxin reductase (the oxidation/reduction partner to Adrenodoxin), requires FAD for activity. The metabolism of glutaric acid requires the FAD-dependent enzyme glutaryl-CoA-dehydrogenase, and as FAD levels decrease glutaric acid in urine increases. Hence, FAD deficiency, such as is common in conditions such as autism, would be accompanied by an increase in the amount of glutaric acid, and the reduced activity of Adrenodoxin reductions and a reduction in the conversion of 25OHD, to 1,25diOHD, with functional vitamin D deficiency, and would correlate with an increase in urinary phosphoric acid (R2 = 0.3794).



Formation of iron-sulphur clusters, such as those seen in adrenodoxin, as well as the formation of intracellular glutathione requires functional vitamin B12. Various markers of functional vitamin B12 sufficiency include MMA (R2 = 0.4274), a marker of Adenosyl B12 insufficiency, and HVA (R2 = 0.4274), and QA (R2 = 0.6102), which all had good correlations with elevated phosphoric acid.

Formation of CoQ10 requires 3 methylation steps, and in methyl B12 deficiency, there is an increase in 3-hydroxymethylglutaric acid, which correlated with increased phosphoric acid levels (lR2 = 0.5602)
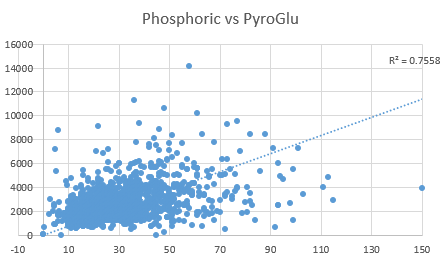
Formation of intracellular glutathione is dependent upon intracellular cysteine levels, which come from processing of dietary methionine to homocysteine, then to cystathionine, and then cysteine. In the absence of sufficient intracellular cysteine, glutamate (used in the formation of glutathione) is rapidly converted to pyroglutamic acid. Urinary glutamic acid levels strongly correlated with urinary phosphoric acid (0.7558). As can be seen from the graphs, there was an increasing rate of correlation between levels of phosphoric acid in urine, and increasing degrees of deficiency of Citrate (iron deficiency), Glutaric acid (Vitamin B2 deficiency), MMA (AdenosylB12 deficiency) and HVA, QA, CoQ10, and PyroGlutamate (Methyl vitamin B12 deficiency). The higher correlation with pyroglutamate levels suggests that problems in the intracellular processing of ferrodoxin are critical to the function of vitamin D3, and as intracellular glutathione is reduced so too the production of ferrodoxin, and the ability to activate vitamin D3. "Adrenodoxin acts together with Adrenodoxin reductase in "helping" CYP27B1 to hydroxylate 25-hydroxy vitamin D and so form 1,25 dihydroxyD (Calcitriol)". Potentially administration of 1,25 diOHD would overcome this problem, however it is not known if there is transport into the brain. The associations outlined above are generally not known even by those working in the field as witnessed by a lead researcher in the field "I am not aware of the associations that you highlight".

Hu etal, 2016


Donayeva etal, 2023
South Korea, autism and the Nexus Theory™
In 2018 the highest incidence of autism was in South Korea with 1 in 30 children being diagnosed with autism. Examination of data on vitamin B12, iron, vitamin B2 and vitamin D, strongly suggest that the Nexus Theory™ would well apply.
Vitamin B12 deficiency is common in S. Korea, with over 17% of S. Koreans having B12 levels of less than 125 pmol/L, and 36.2% having between 125 to 250 pmol/L (Kim etal, 2018).
Studies on dietary intake of riboflavin has shown that one-third of S. Korean adults has an inadequate riboflavin intake (Choi, etal, 2015).
Iron deficiency is also common in S. Korea, with 33% of Koreans 18-49 yo being iron deficient, as judged by ferritin below 15 ug/L, (for females, the mean ferritin in this age group was 30 ug/L, which is below the mean in India) BUT, if one considers that you can see iron deficiency metabolically when ferritin is below 70, this would mean that the vast majority of women of child bearing ages would be iron deficient.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3924001/
Adding to the picture, and completing the requirements of Nexus Theory, in 2014, 82.5% of S. Korean females were deemed to be vitamin D deficient (Park etal, 2018), an increase from 28.2% in 2008.
References/ Useful links.
-
Ali, Asad, Cui, Xiaoying and Eyles, Darryl (2016). Developmental vitamin D deficiency and autism: putative pathogenic mechanisms. Journal of Steroid Biochemistry and Molecular Biology, . doi:10.1016/j.jsbmb.2016.12.018
-
Adam Zalewski, Nina S. Ma, Balazs Legeza, Nora Renthal, Christa E. Flück, Amit V. Pandey, Vitamin D-Dependent Rickets Type 1 Caused by Mutations in CYP27B1 Affecting Protein Interactions With Adrenodoxin, The Journal of Clinical Endocrinology & Metabolism, Volume 101, Issue 9, 1 September 2016, Pages 3409–3418, https://doi.org/10.1210/jc.2016-2124
-
Vinkhuyzen, A. A. E., Eyles, D. W., Burne, T. H. J., Blanken, L. M. E., Kruithof, C. J., Verhulst, F., Jaddoe, V. W., Tiemeier, H. and McGrath, J. J. (2016). Gestational vitamin D deficiency and autism-related traits: the Generation R Study. Molecular Psychiatry, . doi:10.1038/mp.2016.213
-
Hu etal 2016 Perinatal iron deficiency-induced hypothyroxinemia impairs early brain development https://www.ncbi.nlm.nih.gov/pubmed/27231981
-
Yu etal, 2015 Iron deficiency, an independent risk factor for isolated hypothyroxinemia in pregnant and non-pregnant women of childbearing age in China. J. Clinic endocrinol and metabolism 100(4), 1594-1601 https://pubmed.ncbi.nlm.nih.gov/25599388/
-
Pertile, Renata A. N., Cui, Xiaoying and Eyles, Darryl W. (2016). Vitamin D signaling and the differentiation of developing dopamine systems. Neuroscience, 333 193–203. doi:10.1016/j.neuroscience.2016.07.02
-
Vuillermot, Stephanie, Luan, Wei, Meyer, Urs and Eyles, Darryl (2017). Vitamin D treatment during pregnancy prevents autism-related phenotypes in a mouse model of maternal immune activation. Molecular Autism, 8 1: . doi:10.1186/s13229-017-0125-0
-
Gazibara, Tatjana, Elbert, Niels J., den Dekker, Herman T., de Jongste, Johan C., Reiss, Irwin, McGrath, John J., Eyles, Darryl W., Burne, Thomas H., Tiemeier, Henning, Jaddoe, Vincent W. V., Pasmans, Suzanne G. M. A. and Duijts, Liesbeth (2016). Associations of maternal and fetal 25-hydroxyvitamin D levels with childhood eczema: The Generation R Study. Pediatric Allergy and Immunology, 27 3: 283–289. doi:10.1111/pai.12530
-
Cairncross, Carolyn, Grant, Cameron, Stonehouse, Welma, Conlon, Cath, McDonald, Barry, Houghton, Lisa, Eyles, Darryl, Camargo, Carlos A., Coad, Jane and von Hurst, Pamela (2016). The relationship between vitamin D status and allergic diseases in New Zealand preschool children. Nutrients, 8 6: . doi:10.3390/nu8060326
-
Miliku, Kozeta, Vinkhuyzen, Anna, Blanken, Laura M. E., McGrath, John J., Eyles, Darryl W., Burne, Thomas H., Hofman, Albert, Tiemeier, Henning, Steegers, Eric A. P., Gaillard, Romy and Jaddoe, Vincent W. V. (2016). Maternal vitamin D concentrations during pregnancy, fetal growth patterns, and risks of adverse birth outcomes. American Journal of Clinical Nutrition, 103 6: 1514–1522. doi:10.3945/ajcn.115.123752
-
Overeem, Kathie, Eyles, Darryl W., McGrath, John J. and Burne, Thomas H. J. (2016). The impact of vitamin D deficiency on behaviour and brain function in rodents. Current Opinion in Behavioral Sciences, 7 47–52. doi:10.1016/j.cobeha.2015.11.012
-
Fernell, Elisabeth, Bejerot, Susanne, Westerlund, Joakim, Miniscalco, Carmela, Simila, Henry, Eyles, Darryl, Gillberg, Christopher and Humble, Mats B. (2015). Autism spectrum disorder and low vitamin D at birth: a sibling control study. Molecular Autism, 6 1: 3.1–3.9. doi:10.1186/2040-2392-6-3
-
Turner, Karly M., Young, Jared W., McGrath, John J., Eyles, Darryl W. and Burne, Thomas H. J. (2013). Cognitive performance and response inhibition in developmentally vitamin D (DVD)-deficient rats. Behavioural Brain Research, 242 1: 47–53. doi:10.1016/j.bbr.2012.12.029
-
Byrne, Jacqueline H., Voogt, Meggie, Turner, Karly M., Eyles, Darryl W., McGrath, John J. and Burne, Thomas H. J. (2013). The impact of adult vitamin D deficiency on behaviour and brain function in male Sprague-Dawley rats. PLoS ONE, 8 8: e71593.1–e71593.14. doi:10.1371/journal.pone.0071593
-
Eyles, D. W., Liu, P. Y., Josh, P. and Cui, X. (2014). Intracellular distribution of the vitamin D receptor in the brain: Comparison with classic target tissues and redistribution with development. Neuroscience, 268 1–9. doi:10.1016/j.neuroscience.2014.02.042
-
Snaidero, N. and Simons, M. 2014 Myelination at a glance. www.jcs.biologists.org/content/joces/127/14/299.full.pdf
-
Mendivil etal, (2017) Melatonin enhances neural stem cell differentiation and engraftment by increasing mitochondrial function. j. Pin. Res, 63 PMID29423196
-
Malczewska-Lenczowska J, Sitkowski D, Surała O, Orysiak J, Szczepańska B, Witek K. The Association between Iron and Vitamin D Status in Female Elite Athletes. Nutrients. 2018 Jan 31;10(2):167. doi: 10.3390/nu10020167. PMID: 29385099; PMCID: PMC5852743.
-
Avino etal, (2018) Neuron numbers increase in the human amygdala from birth to adulthood, but not in autism. PNAS PMID29559529
-
Altun etal, 2018 The Levels of Vitamin D, Vitamin D Receptor, Homocysteine and Complex B Vitamin in Children with Autism Spectrum Disorders. Clin Psychopharmacol Neurosci. 2018 Nov 30;16(4):383-390. doi: 10.9758/cpn.2018.16.4.383.
-
Donayeva A, Kulzhanova D, Amanzholkyzy A, Abdelazim IA, Abilov T, Baubekov Z, Samaha II. Relationship between vitamin D and adolescents' hypothyroidism - a cross-sectional study. Prz Menopauzalny. 2023 Dec;22(4):186-190. doi: 10.5114/pm.2023.133280. Epub 2023 Nov 29. PMID: 38239402; PMCID: PMC10793608.
-
Kim etal, 2018. One-half of Korean adults studied had marginal vitamin B12 status assessed by plasma vitamin B12. Nutr. Res. 50: 37-43
-
Russell-Jones, GJ. Altered Metabolism of Iron, Vitamin B, and Vitamin B12 Potentially Interfere with Vitamin D- Activation in Children with Autism. J Med - Clin Res & Rev. 2024a; 8(5): 1-6.
Russell-Jones GJ. Complex interaction between iron, vitamin B2, vitamin B12 and vitamin D during the activation of vitamin D. J Med - Clin Res & Rev. 2024b; 8(6); 1-5
-
Park etal, 2018 Vitamin D status in South Korean population: Seven-year trend from the KNHANES https://ncbi.nlm.nih.gov/pubmed/29952942
-
Choi etal, 2015 Evaluation of riboflavin intakes and status of 20-64 year old adults in South Korea. Nutrients, 7, 253-264
Special Thanks
Special thanks to www.protopedia.org for the animated GIF images
Copyright © 2018 B12 Oils. All Rights Reserved.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited